Due to unforeseen operational difficulties, orders placed today may not be dispatched until Monday. We apologise for any inconvenience.
The gut lining is like the gatekeeper of your digestive system, a thin layer of cells that allows nutrients and water into the bloodstream while keeping harmful substances like toxins and pathogenic bacteria out. But what happens when this barrier is compromised? You probably have heard the term “leaky gut,” but do you know what that means and how it impacts your gut and overall health?
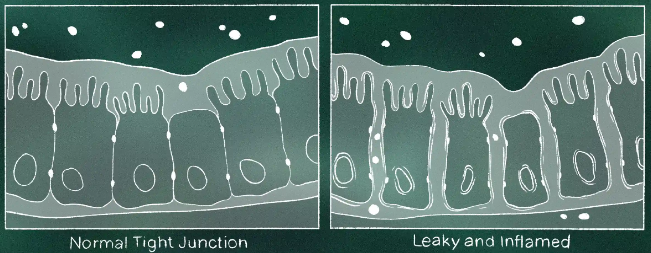
The gut lining consists of a single layer of cells that forms a protective barrier between the external environment and the internal environment of the body. These cells are held together by tight junctions, which regulate the permeability of the gut. In a healthy gut, the tight junctions selectively allow nutrients and water to pass through the gut wall into the bloodstream, while blocking potentially harmful substances, such as toxins, pathogenic bacteria and undigested food particles.
When gut health is compromised, the tight junctions can become weak, leading to increased gut permeability, which allows harmful substances to pass through into the bloodstream. When that happens, your immune system goes into overdrive, trying to defend your body against foreign invaders. This is a protective mechanism, after all your immune system exists to protect you and keep you alive. The problem is that chronic stimulation of the immune system can lead to low-grade inflammation, and over time this chronic inflammation can contribute to the development of various conditions, including autoimmune diseases, metabolic disorders, and gastrointestinal conditions.
In my private nutrition practice, I have been working with clients on improving their gut health for years, specialising in conditions such as Irritable Bowel Syndrome (IBS) and Small Intestinal Bacterial Overgrowth (SIBO). Regardless of the condition I am dealing with, repairing the gut lining is a pivotal part of my gut health protocols, as that is a key element for long-term success.
From clinical experience, I know that when the gut barrier becomes compromised, it doesn’t just affect the digestive system, it can also trigger a whole host of other issues. Clients often come to see me with symptoms that, at first, seem unrelated to the gut-brain fog, skin rashes, fatigue, mood disorders – but when we take a deeper look, we find that increased gut permeability is one of the contributing factors to how they feel. Needless to say, digestive symptoms like persistent bloating, abdominal distention, and irregular bowel movements are almost always present.
Some of the most common symptoms I see in my clinic associated with leaky gut include:
● Digestive issues such as bloating, diarrhoea, constipation, or a combination of both
● Multiple food sensitivities and intolerances
● Chronic fatigue and low energy levels
● Joint pain and muscle aches
● Skin problems such as eczema, acne and allergies
● Cognitive issues, such as brain fog and difficulty concentrating
● Mood disorders such as anxiety and depression
It is important to highlight that leaky gut is often one of many factors that contribute to the symptoms mentioned above. Due to the overlap with other conditions, working with a healthcare professional and ruling out medical conditions is essential.
When I explain increased gut permeability to my clients, one of the first questions I get asked is “what causes it?” – I would love to be able to say there is a single factor that contributes to its development, however, like most health-related conditions, there isn’t a single factor that contributes to increased gut permeability, but a combination of multiple factors:
● Poor diet: a diet low in fibre and high in processed foods, refined sugars, and trans fats can lead to inflammation in the gut and weaken the gut barrier.
● Chronic stress: the gut and the brain are intrinsically connected and chronic stress can impact gut health by altering the composition of the gut microbiota and weakening the gut barrier.
● Medications: nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can damage the gut lining over time. Antibiotics, while necessary in some cases, can disrupt the balance of gut bacteria, leading to inflammation and compromised barrier function.
● Gut dysbiosis: the gut microbiota plays an essential role in maintaining a strong gut barrier. Dysbiosis, or an imbalance of beneficial and opportunistic gut bacteria, is associated with increased gut permeability and inflammation.
● Environmental toxins: exposure to environmental toxins such as pesticides, heavy metals, and pollutants can also damage the gut lining.
At this point you may be asking yourself what can be done to improve increased gut permeability. Just like multiple factors can contribute to it, there isn’t a magic bullet to fix it. The good news is that there are few science-based strategies to support gut lining repair:
● Fibre-rich diet: one of the most important steps you can take to support gut health is to eat a high fibre diet. Fibre not only feeds the beneficial bacteria in your gut but also plays an important role in the production of short-chain fatty acids (SCFAs). SCFAs, particularly butyrate, serve as an energy source for the cells that line the gut, helping to strengthen the gut barrier, reduce inflammation, and support the integrity of the tight junctions.
● Prebiotics: Prebiotics, which are fibres that feed these beneficial bacteria, support a healthy microbiome. Foods like garlic, onions, asparagus, and green bananas are rich sources of prebiotics.
● Stress management: reducing stress is easier said than done, but it is a must when trying to improve gut health. Incorporating stress-reducing activities such as yoga, meditation, and mindfulness practices have been scientifically proven to help.
● Nutraceutical support
Targeted supplementation, alongside dietary and lifestyle modifications, can help speed up gut lining repair. Scientifically proven supplements include:
● L-Glutamine: l-glutamine is an amino acid that serves as a primary fuel source for the cells of the gut lining. Studies have shown that L-glutamine supplementation can support gut barrier integrity and reduce permeability.
● Zinc carnosine: this form of zinc has been shown to promote gut healing by strengthening the gut barrier and reducing inflammation.
● Vitamin D: low levels of vitamin D are associated with increased gut permeability.
I always check my clients’ levels and recommend supplementation if needed.
● Omega-3 fatty acids: omega-3 fatty acids, specifically EPA and DHA found in fish oils, have potent anti-inflammatory effects.
● Colostrum: bovine colostrum contains a variety of beneficial compounds that have been shown to support gut barrier function and reduce gut permeability.
● ION* Gut + Microbiome: As leaky gut is ultimately the widening of natural gaps and formation within the intestinal walls, finding a natural solution that retightens those tight junctions is key.

The topic of leaky gut is becoming more well acknowledged, and due to scientific research we now know it has significant consequences that extend beyond our gut health. If you think increased gut permeability may be contributing to your health symptoms, get in touch – my 16-week signature gut health programme is a science-backed approach to overcoming chronic digestive symptoms that is completely tailored to you. With The Gutfulness Method, you will finally understand what’s causing your symptoms and take control of your digestive health. About the author: Marilia Chamon is a London-based gut health specialist, registered nutritional therapist, and the founder of Gutfulness Nutrition. Marilia has undergone extensive training on the pathophysiology of IBS in addition to completing the Monash University ‘Low FODMAP Diet for IBS’ training course for health professionals. A SIBO Approved Practitioner and certified in Applying Functional Medicine in Clinical Practice from the world renowned Institute For Functional Medicine (IFM), she is the creator of The Gutfulness Method, a 16-week personalised gut health programme designed to help individuals overcome chronic digestive symptoms.
Written by Marilia Chamon
Registered Nutritional Therapist
Founder of Gutfulness Nutrition
Instagram @gutfulnessnutrition
Share this article